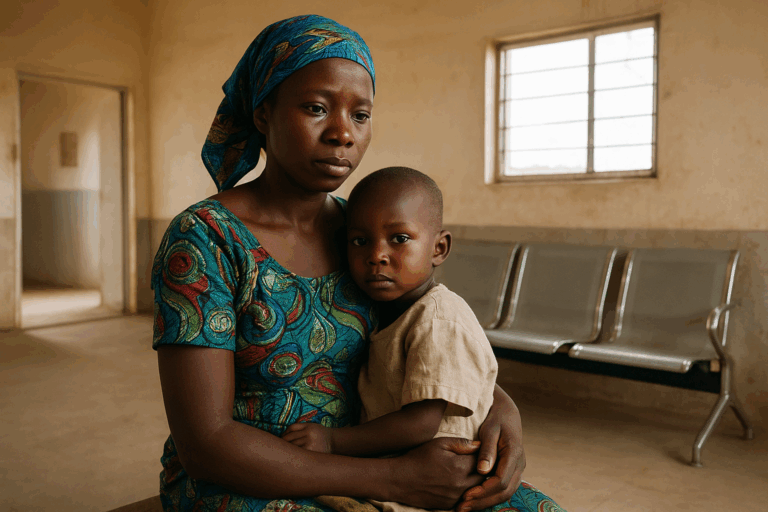
The UK The pandemic has put a magnifying glass over the disparities in treatment between socioeconomic groups. It has brought to the forefront that those living in England’s most deprived areas experience poorer health outcomes than those living in wealthy areas.
A breakthrough report found that the coronavirus death rate in Greater Manchester was 25% higher than the average for all of England between January and March this year, leading to decreases in life expectancy and widening social and health inequalities across the northwest of England over the past year.
This trend has worrying implications for coronary heart disease (CHD), which causes approximately 25% of all deaths in the UK each year, according to the British Heart Foundation. CHD rates in the most vulnerable 10% of the population are twice as high as in the least deprived area.
However, there is room for hope, as the pandemic also unearthed a solution to help address these shortcomings in delivering care: technology.
Consistent patient experience
When it comes to heart health, the NHS has taken a major step towards democratising care. First, it identified a new patient pathway for the diagnosis of CHD, shifting to a CT-first approach, rather than the traditional stress testing method.
More recently, the NHS mandated that all NHS hospitals must adopt a range of new technologies as part of the diagnosis and treatment of CHD. One of these technologies is the artificial intelligence-powered HeartFlow Analysis, which is a non-invasive technology that applies deep learning algorithms to data from a CT scan, alongside input from highly trained analysts, to create a digital, personalised 3D model of the heart.
Adding the HeartFlow Analysis after a CT scan gives clinicians an even greater level of insight into what’s happening in their patients’ arteries and helps reduce the number of repeat tests and avoidable invasive procedures. This approach means the NHS can standardise the patient experience and level of care during the diagnostic phase across the country. The aim is that a patient in Chelsea will have exactly the same diagnostic experience and level of care as a patient in Blackpool.
Less time in hospital
The pandemic also forced a reduction in available time for healthcare. Whereas those in secure employment are able to maintain their income while away from work, for either holiday or illness, those in temporary work, such as zero-hours contracts, freelancers, or those in the gig economy, are not. Therefore, a critical learning from the past two years is the necessity to minimise any unnecessary time patients spend in the hospital.
Using technology to improve patient pathways is one route to success. Technologies like the HeartFlow Analysis can be ordered by a physician without requiring a patient to be in the office other than for the initial CT scan. The information provided by the HeartFlow Analysis helps medical professionals triage patients and identify those with severe diseases who are in urgent need of intervention, such as stenting. It also helps to identify patients who can be safely managed with medication alone and don’t need to stay on waiting lists for further investigations. Being able to efficiently stratify patients helps reduce unnecessary time in the hospital, and may improve the efficiency of care delivery, which in turn may help reduce backlogs created by the pandemic.
Recognising bias
The pandemic has also brought more attention to biases that exist in society – whether they’re along the lines of class, gender or race.
The topic of gender was explored in HeartFlow’s research into cardiac care, which found that one in eight women (13%) feel ignored when presenting symptoms of heart disease to healthcare professionals, compared to just 4% of men. And of UK adults who have received a CHD diagnosis, women experiencing symptoms were 55% more likely than men to visit the doctor multiple times before receiving a referral for further investigation. On top of this, women are five times more likely to receive a false finding from the cardiac stress tests that are traditionally used to assess heart health.
These historical diagnostic pathways rely on substantial subjectivity in interpretation, as well as identifying characteristics of a given patient which may contribute to these biases in CHD diagnosis. In contrast, AI-enabled technologies that can be conducted without knowledge of the specific demographics of a given patient makes the diagnosis solely about the condition and may mitigate the risk of unconscious bias resulting in better care for all patients.
In summary
The pandemic has been incredibly challenging for healthcare, but it has forced foundations to be laid which can result in a future service that provides for all members of society equitably. The continued development and improvement of medical technologies, in particular AI applications, will be an important tool in delivering that service in the UK and beyond.

Charles Taylor is the founder and Chief Technology Officer at Heartflow.